Male Urinary Incontinence Treatment in San Antonio, TX
Urge incontinence in men can be attributed to a variety of underlying causes that disrupt normal bladder function. One common cause is Benign Prostatic Hyperplasia (BPH), where an enlarged prostate obstructs urine flow and irritates the bladder. Neurological disorders such as Parkinson’s disease, multiple sclerosis, and stroke can also impair nerve signals that control the bladder, leading to involuntary contractions. Infections or inflammation of the bladder, such as cystitis, can cause increased bladder sensitivity and urgency. Additionally, certain medications, especially diuretics and drugs that affect bladder control, can exacerbate urge incontinence. Lifestyle factors like excessive caffeine or alcohol intake may irritate the bladder and contribute to urgency. Understanding these diverse causes is essential for effectively diagnosing and managing urge incontinence in men.
Radiation therapy for prostate cancer, a common and effective treatment option, can also sometimes lead to urge incontinence. This condition occurs when the radiation damages the tissues and nerves surrounding the prostate and bladder. The irritation and inflammation caused by radiation can reduce the bladder’s capacity to hold urine and impair the control mechanisms of the urinary sphincter. Consequently, patients may experience a sudden and intense urge to urinate, often leading to involuntary leakage before reaching the bathroom.
Benign Prostatic Hyperplasia (BPH), a common condition in aging men, can lead to urge incontinence by causing the prostate gland to enlarge and press against the urethra. This pressure obstructs the normal flow of urine, making it difficult for the bladder to empty completely. As a result, the bladder becomes overactive and more sensitive, often contracting involuntarily in an attempt to expel urine, which triggers a sudden and intense urge to urinate. This urgency can be so strong that it leads to involuntary leakage before the person can reach the bathroom. Sometimes even after treatment of BPH, urge incontinence continues to be an issue due to bladder changes created by chronic obstruction.
What is Axonics Therapy?
Axonics Therapy is a clinically proven solution for treating symptoms of overactive bladder (including urinary urgency incontinence), bowel (fecal) incontinence and urinary retention.1
What are the benefits of Axonics Therapy?
Small Size: Safely delivers therapy with a miniaturized implant
- Long-Term Therapy: Designed to provide long-term symptom relief
- Full-Body MRI: Eligible for full-body MRI under approved conditions
- Clinically Proven: In a clinical study, Axonics Therapy provided sustained safety and symptom relief at 3 years2
How does Axonics Therapy work?

The Evaluation Step: To see if Axonics Therapy is right for you, you will undergo a short period of therapy using a temporary system. The evaluation period allows you to experience the level of symptom relief the therapy may provide before you commit to long-term therapy.
Long-term Therapy: If you and your doctor determine that Axonics Therapy is right for you, you will have an outpatient procedure where the miniaturized Axonics implant is placed just beneath the skin in the upper part of your buttock.
Clinically Proven. Patient Approved.
Backed by clinical studies, Axonics Therapy is clinically proven to help regain bladder and bowel control and deliver clinically meaningful improvement in quality of life.
At 1-Year,
- 93% of patients were satisfied with their therapy1
- 89% of patients experienced a ≥50% reduction in urinary urgency incontinence symptoms1
- <2% of patients reported discomfort at the implant site1
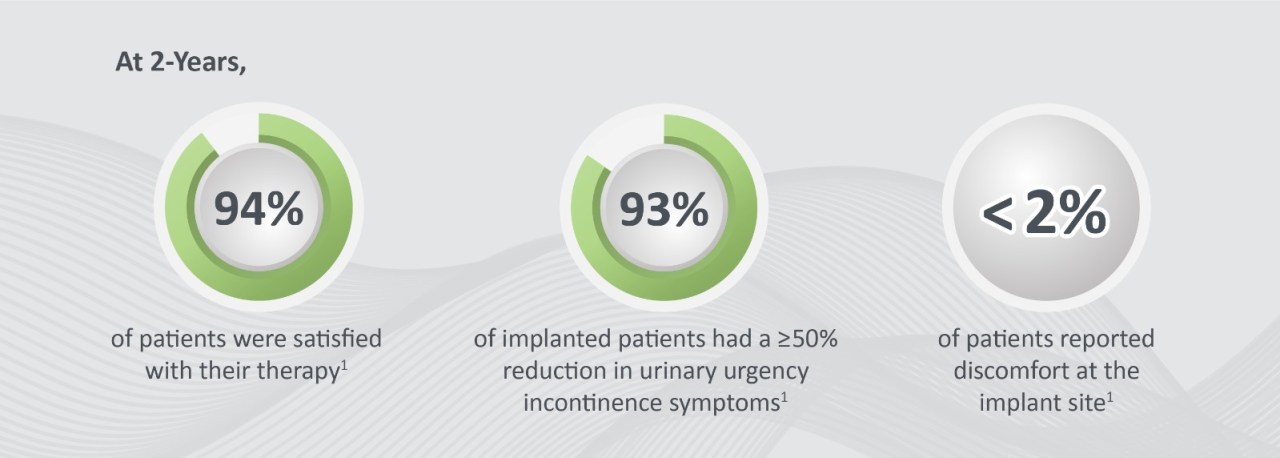
At 2-Years,
- 94% of patients were satisfied with their therapy1
- 93% of patients experienced a ≥50% reduction in urinary urgency incontinence symptoms1
- <2% of patients reported discomfort at the implant site1
Disclaimer: Results and experiences may vary.
Who is a good candidate for Axonics Therapy?
It is up to you and your healthcare provider to determine if you are a good candidate for Axonics Therapy.
Axonics Therapy is an approved treatment for patients suffering with:
- Overactive bladder (OAB) – the urgent need to urinate which may result in frequent urination and/or incontinence (leakage) episodes
- Urinary frequency – the need to urinate 8 or more times a day, which may or may not be associated with urgency
- Urinary urgency incontinence (UUI) – the urgent need to urinate or trouble holding urine before making it to the restroom
- Fecal (bowel) incontinence – involuntary loss of stool which may or may not be associated with urgency
- Nonobstructive urinary retention (UR) – the inability to completely empty the bladder which may result in trouble urinating or frequent small voids
- Axonics Therapy is indicated for patients who have failed conservative treatments, such as lifestyle changes, physical therapy, or medications
Get the symptom relief you deserve!
Important Safety Information:
Implantation and use of the Axonics System incurs risk beyond those normally associated with surgery, some of which may necessitate surgical intervention.
Results and experiences may vary and are unique to each patient. No promise or guarantee is made about specific results or experiences. Talk to your doctor about whether the Axonics System is right for you and to discuss the potential risks and benefits. For more information about safety and potential risks, go to: www.axonics.com/isi.
Caution: Federal law (USA) restricts this device to sale and use by, or on the order of, a physician.
1. Pezzella A, et al. Neurourol Urodyn. 2021
2. Blok, B, et al. Neurourol Urodyn. 2020)

 Small Size: Safely delivers therapy with a miniaturized implant
Small Size: Safely delivers therapy with a miniaturized implant